Urinalysis dipstick testing is a rapid, non-invasive method for detecting urinary tract infections (UTIs) and kidney-related abnormalities. It measures physical and chemical parameters, providing critical insights for diagnosis and treatment plans.
1.1 Overview of Urinalysis and Its Importance
Urinalysis is a fundamental diagnostic tool for assessing urinary tract infections (UTIs), kidney function, and metabolic disorders. It provides insights into physical and chemical properties of urine, aiding in early detection of abnormalities. Regular urinalysis is crucial for monitoring chronic conditions, ensuring timely interventions, and maintaining patient health. Its non-invasive nature makes it a cornerstone in clinical practice;
1.2 Role of Dipstick Testing in Clinical Practice
Dipstick testing is a cornerstone in clinical practice, offering rapid and reliable assessment of urinary abnormalities. It detects infections, kidney issues, and metabolic disorders, guiding timely interventions. Widely used in primary care, it enables early diagnosis and monitoring, ensuring effective treatment plans and improved patient outcomes. Its convenience and accuracy make it indispensable for routine and specialized medical evaluations.
Understanding Urinalysis Dipstick Components
Urinalysis dipsticks consist of pads coated with chemicals that react to specific urinary components. They measure physical traits like color and clarity, as well as chemical parameters such as glucose and protein, aiding in the detection of various health conditions.
2.1 Physical Characteristics Measured by Dipsticks
Dipsticks measure physical characteristics such as urine color, clarity, and specific gravity. These assessments provide insights into hydration levels and potential kidney function issues. Color changes indicate possible abnormalities like jaundice or blood presence. Clarity helps detect infections or kidney stones. Specific gravity measures urine concentration, reflecting the body’s ability to regulate fluids.
2.2 Chemical Parameters Assessed by Dipsticks
Dipsticks assess chemical parameters like pH, protein, glucose, ketones, blood, bilirubin, urobilinogen, nitrite, and leukocyte esterase. These tests help detect conditions such as diabetes, kidney damage, infections, or liver issues. Positive results for blood or protein may indicate urinary tract infections or chronic kidney disease, guiding further diagnostic steps and treatment plans effectively.

Clinical Significance of Urinalysis Results
Urinalysis results are crucial for early detection of urinary tract infections, kidney dysfunction, and metabolic disorders, guiding timely interventions and improving patient outcomes significantly.
3.1 Common Abnormalities Detected by Dipsticks
Dipstick testing commonly identifies abnormalities such as leukocytes, nitrites, proteinuria, hematuria, and glucose in urine, indicating potential urinary tract infections, kidney dysfunction, or metabolic disorders. These findings are critical for early detection and monitoring of conditions like UTIs, diabetic nephropathy, and acute kidney injury, enabling timely clinical interventions and improving patient outcomes significantly.
3.2 Implications for Diagnosis and Treatment
Positive dipstick results for abnormalities like proteinuria or hematuria often prompt further diagnostic testing, such as urine culture or imaging. These findings guide targeted therapies, including antibiotics for UTIs or referrals for nephrology evaluation. Accurate documentation ensures continuity of care, enabling healthcare providers to monitor progression and adjust treatment plans effectively, thereby improving patient outcomes and reducing complications.
How to Read and Interpret Urinalysis Dipstick Results
Match dipstick color changes to reference charts, noting deviations from normal ranges. Ensure timely reading to avoid false results from prolonged exposure to air or contaminants.
4.1 Colorimetric Scale and Result Interpretation
The colorimetric scale on urinalysis dipsticks provides a visual guide for interpreting results. Each parameter, such as pH, protein, or blood, corresponds to a specific color change. Results are compared to reference charts to determine normal or abnormal levels. Timing is critical, as prolonged exposure to air can alter readings. Accurate interpretation ensures reliable clinical insights for diagnosing conditions like UTIs or kidney dysfunction.
4.2 Common Interferences and False Results
Urinalysis dipstick results can be affected by various factors, such as contamination, improper storage, or exposure to light. Substances like medications, food, or menstrual blood may cause false positives or negatives. For instance, quaternary ammonium compounds can inhibit enzyme reactions, while prolonged air exposure may alter pH readings. Understanding these interferences is crucial for accurate interpretation and reliable clinical decision-making.
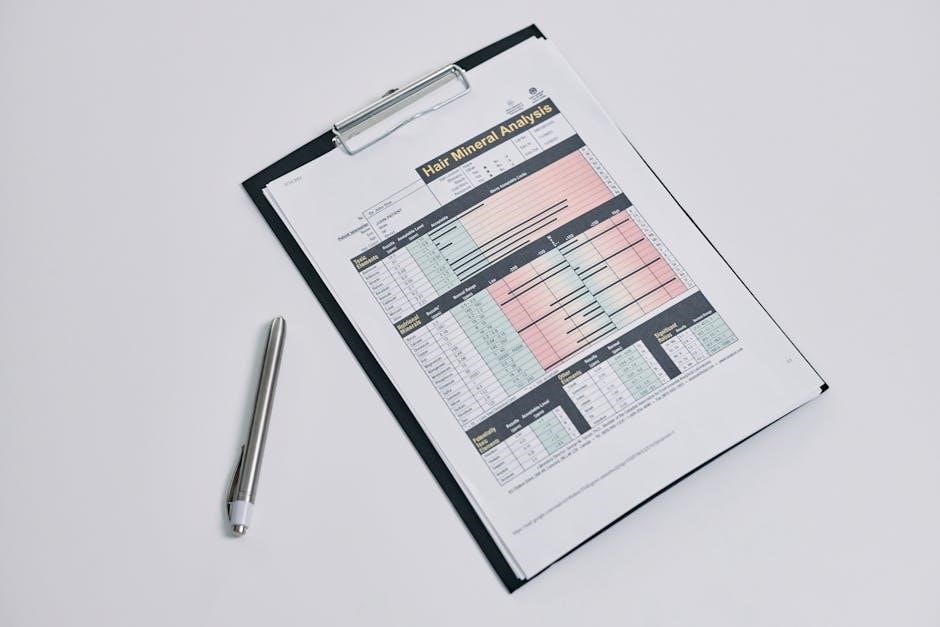
Urinalysis Dipstick Results Form PDF: Structure and Content
The form includes sections for patient demographics, test date, and results of physical and chemical parameters measured by dipsticks, ensuring standardized documentation and clarity.
5.1 Standardized Format for Recording Results
The urinalysis dipstick results form includes patient demographics, test date, and sections for physical and chemical parameters. It features fillable fields, checkboxes, and color-coded scales for clarity. This standardized format ensures consistency, reducing interpretation errors and facilitating accurate documentation. The structure is designed to be user-friendly, with clear headings and organized data presentation, aiding healthcare providers in quick decision-making and maintaining precise records for future reference.
5.2 Key Fields and Information Included in the Form
The form includes patient identification, date, urine characteristics, and test results for parameters like pH, protein, glucose, ketones, blood, leukocytes, and nitrites. It also features sections for visual observations and additional notes. This comprehensive structure ensures all necessary data is captured, aiding in accurate diagnosis and treatment planning, while maintaining clear and organized records for healthcare providers to reference.
Clinical Correlations of Dipstick Results
Dipstick results correlate with patient symptoms, aiding in diagnosing conditions like UTIs and kidney disease. Abnormalities in parameters such as pH, protein, and blood guide clinical decisions.
6.1 Correlating Dipstick Findings with Patient Symptoms
Dipstick results are interpreted alongside patient symptoms to identify conditions like UTIs or kidney disease. Positive findings for leukocytes, nitrites, or blood correlate with symptoms such as dysuria, flank pain, or hematuria. Elevated protein levels may indicate nephrotic syndrome, while glucose detection suggests uncontrolled diabetes. Accurate correlation aids in targeted diagnostic workups and personalized treatment plans, ensuring effective patient care and outcomes.
6.2 Differentiating Between Benign and Pathological Conditions
Dipstick findings help distinguish between benign conditions, such as dehydration or transient proteinuria, and pathological states like kidney disease or UTIs. For instance, trace proteinuria may be normal, while significant levels indicate nephropathy. Blood detection could suggest benign hematuria or severe conditions like stones or cancer. Accurate interpretation ensures proper differentiation, guiding further diagnostic steps and appropriate management strategies.

Troubleshooting Urinalysis Dipstick Results
Common issues include false positives due to contamination or improper technique. Resolving these involves ensuring accurate sample collection, using controls, and adhering to manufacturer guidelines for dipstick testing.
7.1 Common Issues in Dipstick Testing
Common issues in dipstick testing include contamination, improper technique, and false results due to interfering substances. Ensuring accurate results requires adherence to manufacturer guidelines, proper sample handling, and minimizing external factors. Standardized procedures and training are essential to mitigate these challenges and ensure reliable urinalysis outcomes. Regular quality control measures can also help identify and address recurring issues effectively.
7.2 Strategies for Ensuring Accurate Results
Accurate dipstick results rely on proper technique, including correct immersion time and reading within the specified timeframe. Using high-quality strips, avoiding contamination, and following manufacturer guidelines are crucial. Staff training and regular quality control checks help maintain consistency. Additionally, documenting results promptly and storing them securely ensures data integrity and traceability for clinical decision-making and patient care.

Comparison with Other Urinalysis Methods
Dipstick testing is quick and cost-effective but less precise than laboratory-based methods. Advanced techniques, like mass spectrometry, offer higher accuracy for complex diagnoses, though they are time-consuming.
8.1 Advantages and Limitations of Dipstick Testing
Dipstick testing offers rapid, cost-effective screening for urinary abnormalities, making it ideal for routine check-ups. However, it lacks the sensitivity of advanced methods like mass spectrometry, potentially missing subtle conditions. Its simplicity also means it’s prone to false results from improper technique or interference, requiring careful handling to ensure accuracy. Despite these limitations, dipsticks remain a valuable diagnostic tool in clinical settings.
8.2 When to Use Advanced Urinalysis Techniques
Advanced urinalysis techniques are recommended when dipstick results indicate persistent abnormalities or when underlying conditions like kidney disease or complex infections are suspected. These methods, such as mass spectrometry, provide deeper insights into proteinuria, hematuria, or metabolic disorders, enabling precise diagnosis and tailored treatment plans. They are essential for cases requiring detailed analysis beyond the scope of dipstick testing.
Documenting and Archiving Urinalysis Results
Accurate documentation ensures reliable patient records and legal compliance. Standardized PDF forms simplify data organization, while secure archiving guarantees long-term accessibility for healthcare providers and future reference needs.
9.1 Importance of Accurate Record Keeping
Accurate record keeping in urinalysis ensures reliable patient care, legal compliance, and traceability of results. It supports clinical decision-making, reduces errors, and enhances patient safety. Standardized PDF forms maintain consistency, facilitating clear communication among healthcare providers and ensuring longitudinal tracking of patient health. Proper documentation also aids in clinical audits and quality improvement initiatives, aligning with regulatory standards and best practices in healthcare settings.
9.2 Best Practices for Storing Urinalysis Results
Store urinalysis results securely using password-protected PDF forms and encrypted digital systems. Ensure accessibility for authorized healthcare providers while maintaining patient confidentiality. Use tamper-proof formats to preserve data integrity. Regularly back up files to prevent data loss. Adhere to HIPAA and other regulatory standards to ensure compliance and protect sensitive medical information effectively.
Best Practices for Using Urinalysis Dipsticks
Handle dipsticks carefully to avoid contamination. Dipsticks should be immersed in urine for the recommended time. Read results within the specified timeframe to ensure accuracy and reliability.
10.1 Proper Technique for Dipstick Testing
Proper dipstick testing involves collecting a midstream urine sample to minimize contamination. Dip the strip into the sample, ensuring all test areas are covered. Avoid touching the test pads with your fingers. Hold the strip horizontally and wait for the specified time before reading results. Use the colorimetric chart provided to interpret the findings accurately.
10.2 Maintaining Quality Control in Dipstick Testing
Quality control in dipstick testing ensures accurate and reliable results. Always check the expiration date of the strips and store them properly. Avoid exposing strips to moisture or extreme temperatures. Use control strips to verify test accuracy. Ensure staff are trained in proper testing techniques and adhere to manufacturer guidelines for optimal performance and result consistency.
Case Studies and Real-World Applications
Urinalysis dipstick testing aids in identifying conditions like UTIs and kidney dysfunction. For instance, the Multistix 10 SG strip detects abnormalities, guiding timely interventions and improving patient outcomes effectively.
11.1 Examples of Dipstick Results in Clinical Scenarios
In clinical practice, urinalysis dipstick results often reveal critical insights. For instance, a patient with symptoms of dysuria and frequent urination may show positive leukocytes and nitrites, indicating a urinary tract infection. Conversely, trace proteinuria in an asymptomatic individual might suggest early kidney dysfunction, prompting further investigation. These examples highlight how dipstick testing aids in timely diagnosis and targeted interventions.
11.2 Lessons Learned from Common Dipstick Results
Common dipstick results, such as positive nitrites or blood, often indicate urinary tract infections or kidney stones. False positives due to contamination or improper technique highlight the need for standardized testing protocols. These insights underscore the importance of accurate interpretation and proper sample collection to ensure reliable results, guiding effective patient care and minimizing unnecessary interventions.
Urinalysis dipstick testing remains a cornerstone in diagnosing urinary tract infections and kidney diseases, offering rapid results. Future advancements may integrate digital health solutions for enhanced accuracy and accessibility.
12.1 Summary of Key Points
Urinalysis dipstick testing is a reliable, cost-effective tool for detecting urinary abnormalities. It measures key parameters like pH, protein, and glucose, aiding in diagnosing conditions such as UTIs and kidney diseases. Accurate results depend on proper technique and interpretation. The urinalysis dipstick results form PDF standardizes documentation, ensuring clarity and consistency for healthcare providers, which is essential for patient care and legal record-keeping purposes.
12.2 Emerging Trends in Urinalysis Testing
Emerging trends in urinalysis testing include advanced dipstick technologies for improved accuracy and the integration of automated readers for faster results. Point-of-care testing solutions are becoming more prevalent, enabling quick and precise diagnosis in clinical settings. These innovations enhance the detection of chronic kidney disease and urinary tract infections, ultimately improving patient outcomes through early intervention and streamlined data management systems.